Learn how FidelityEHR electronic health record software supports EDI, Authorization & Billing:
EDI (Electronic Data Interchange)
FidelityEHR uses embedded health information exchange (HIE) technology to mobilize, transmit and consume health record information electronically across data systems to support client care coordination.
FidelityEHR allows the administrative User select to exchange or transfer relevant data between sources through manual command execution, on a schedule basis, through a predetermined automated exchange process or in real-time, depending on your data needs.
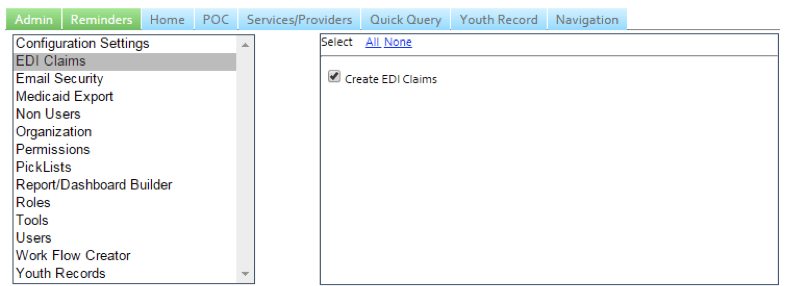
Access to the Medicaid Export and EDI submission features are permissions-driven and established by each User role. Permissions for these features can be set within the Administration Site or within a configuration.
Role-based Permission for EDI Claims Access
FidelityEHR also has multiple mechanisms for exchanging data with other stakeholders such as SAMSHA for reporting purposes, with other electronic health record systems and for relevant provider groups.
Authorization & Billing
FidelityEHR is uniquely able to support billing, authorization and electronic claims adjudication for Systems of Care. Billable services are tied to strategies within the Plan of Care, enable collaborative care coordination with multiple providers and support multiple funding sources. Threshold criteria for claim submissions are defined by the Configuration Administrator in the user interface via the Admin Settings. In addition, the solution has the ability to provide insurance eligibility checks.
Claims are derived directly from services provided to clients/youth/families. Billable services are attached to Service Notes, Youth Need Strategies and Strategy Tasks, and Crisis Plan Action Steps and Action Step Tasks. All of these are reflected in the Plan of Care with the exception of Service Notes.
Adding/Editing Service Information within the POC
Billable Services within Service Notes
FidelityEHR supports auto assessment of claims ready for adjudication. The different stages are Ready to Submit, Submitted with no Response, Response Received but claim not paid, Claim Paid, and Do Not Send (excluded by client or system thresholds as unadjudicatable). Configuration Administrator-level Users can navigate through the EDI Claims user interface to view claims in various stages.
Automate billing
The system creates 837 line items automatically from the information in the Youth Record and Service Note. FidelityEHR has experience meeting payee requirements for multiple Medicaid and non-Medicaid trading partners, and will configure each of the payee trading partners during the implementation process.
Logs are kept for the submission and response receipt process. All adjudicated claims have a record of where they are in the process, and once paid, are automatically updated as Paid in the system, with this showing in the UI.
FidelityEHR can bill and receive payments for all billable services and provide a comparison with authorized services for each provider. The system can identify multiple payers on a single date and generate a file for consumption by an AP system to generate provider payment. The system supports multiple payors and supports electronic generation of claims files for billable services in predefined formats for submission to payors.
Billable Need Strategies, Tasks, and Crisis Plan Action Steps and Tasks can be created for Family Members and authorized within the POC. The service delivery for the Family Member is tracked within the POC and is capable of being submitted for payment through the EDI Claims functionality.
Authorized Billable Services